When someone’s having a mental health crisis, every minute matters. But too often, families end up lost in a broken system when they need help the most.
Right now, nearly 1 in 10 ER visits is for mental health issues, mostly because people can’t get appointments with mental health professionals when they need it. With limited options, families in crisis will struggle for weeks while their loved one suffers or they rush to an ER that’s built for heart attacks, not panic attacks.
What Good Crisis Care Looks Like
The best crisis systems have three parts: someone to talk to (like 988), someone who comes to help (mobile crisis teams), and somewhere safe to go if needed. When this works right:
- Help is immediate: Talk to someone trained in crisis support
- Help comes to you: Mobile teams meet people wherever they are currently
- Help continues in a safe space: Stabilization services in a calming environment provide immediate treatment and support, plus prevention services to reduce future crises
Why This Matters
Research shows good crisis care cuts down on return ER visits, shorter hospital stays, and better outcomes for patients. But here’s what that really means: a parent doesn’t have to choose between calling 911 or hoping their kid makes it through the night. A college student having their first panic attack gets real help, not just “call your doctor next week.”
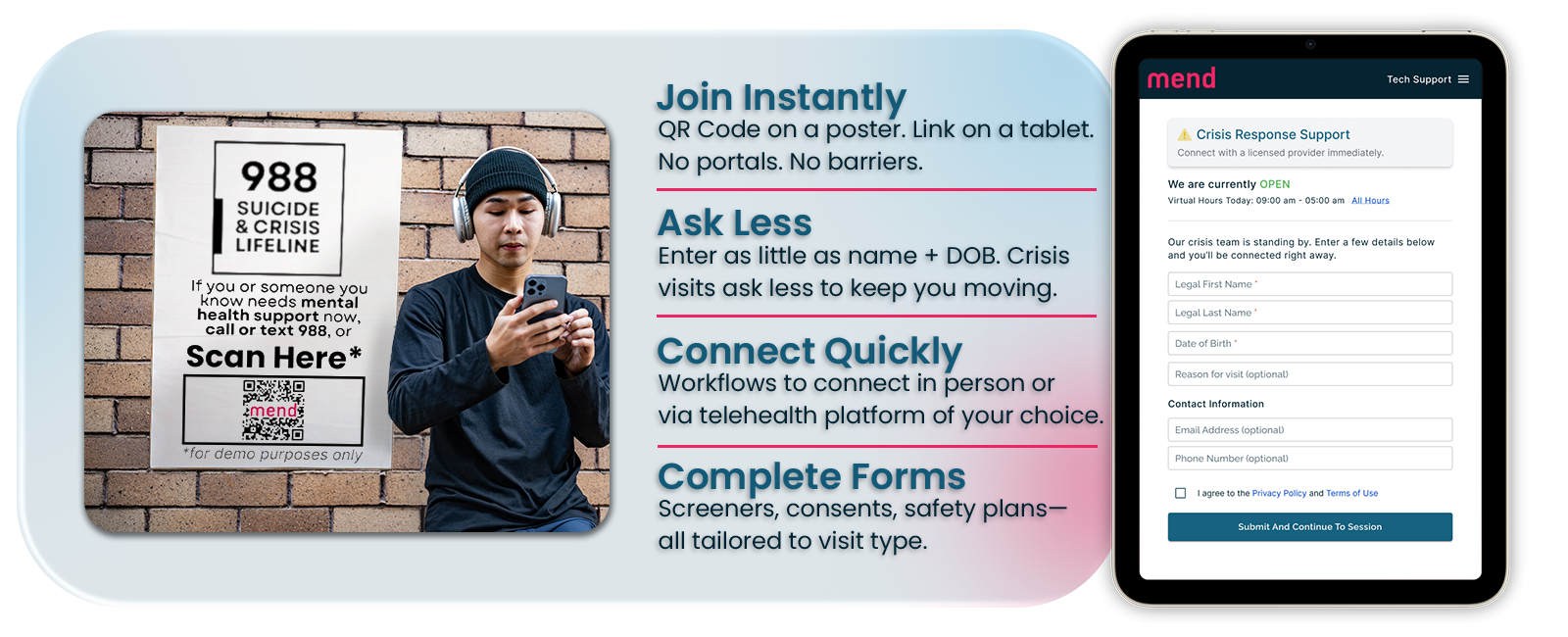
Where Technology Helps
Crisis care only works when everyone’s connected. The person in crisis, their family, crisis workers, and follow-up services all need to communicate seamlessly. That’s where smart healthcare technology comes in. Current technology has the ability to:
- Connect families instantly to the right resources
- Make sure important information follows the person through their care
- Give clear next steps instead of leaving families to figure it out alone
- Let crisis workers focus on helping people, not paperwork
The Bottom Line
Every family should know that when a crisis hits, there’s a clear path to help. Every person in crisis deserves care that meets them where they are. Every healthcare worker deserves tools that make coordinated crisis care actually work.
That’s what we’re building at Mend: technology that doesn’t just manage crisis care, but makes it work better for the people who need it most.
Crisis support is available 24/7 at 988 (call, text, or chat at 988lifeline.org).