Why You Need to Switch to HIPAA Compliant Telehealth, NOW

Privacy is one of the most important parts of a patient’s healthcare experience. Disclosing protected health information (PHI) can cause serious harm to a patient’s safety, personal life, and state of mind. Data breaches or mishandling can also put a practice at serious risk of legal and financial trouble. That is why it is essential to adopt a HIPAA compliant telehealth program when offering virtual care services.
Providers have an immense legal and ethical duty to safeguard PHI. Keeping PHI secure is the main goal of the Health Insurance Portability and Accountability Act (HIPAA). HIPAA protects patients by limiting who can access PHI, when they can access it, and how they use it. Under HIPAA, there can be steep penalties for breaches involving PHI. When it comes to telehealth, all HIPAA compliant entities in the healthcare industry must practice caution and discretion in how they handle patient data.
The Impact of Healthcare Data Breaches
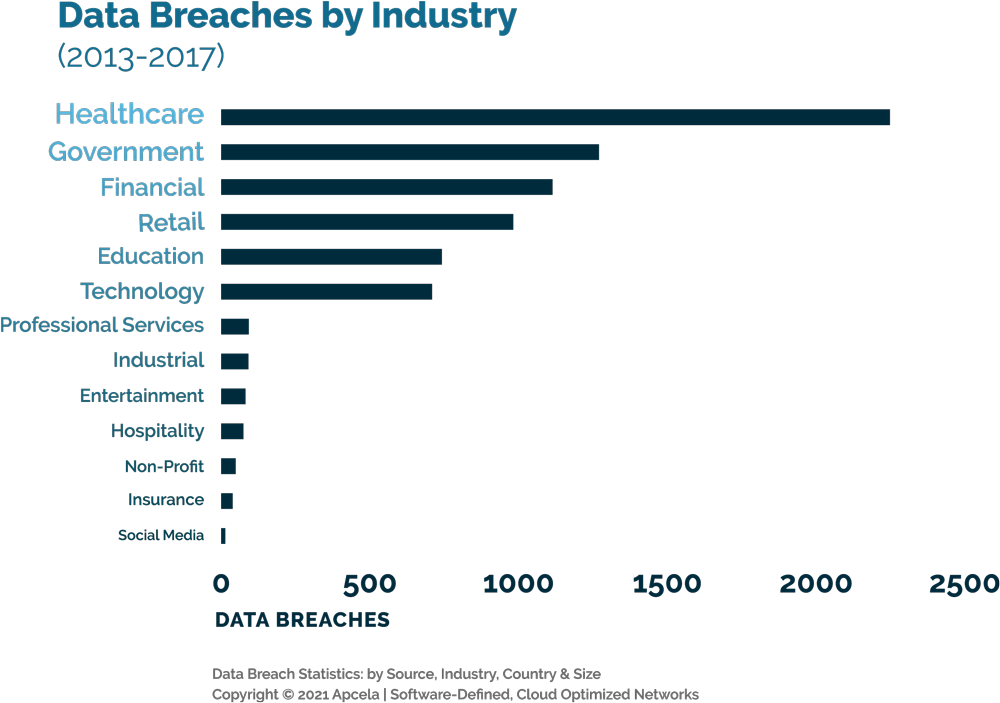
The healthcare industry faces more data breaches than any other sector. Studies show that health data breaches have affected over 250 million Americans since 2010. Healthcare is more digital than ever. That includes the storage of health records and care delivery. Likewise, there are more chances for breaches than ever, whether they are intentional or due to human error.
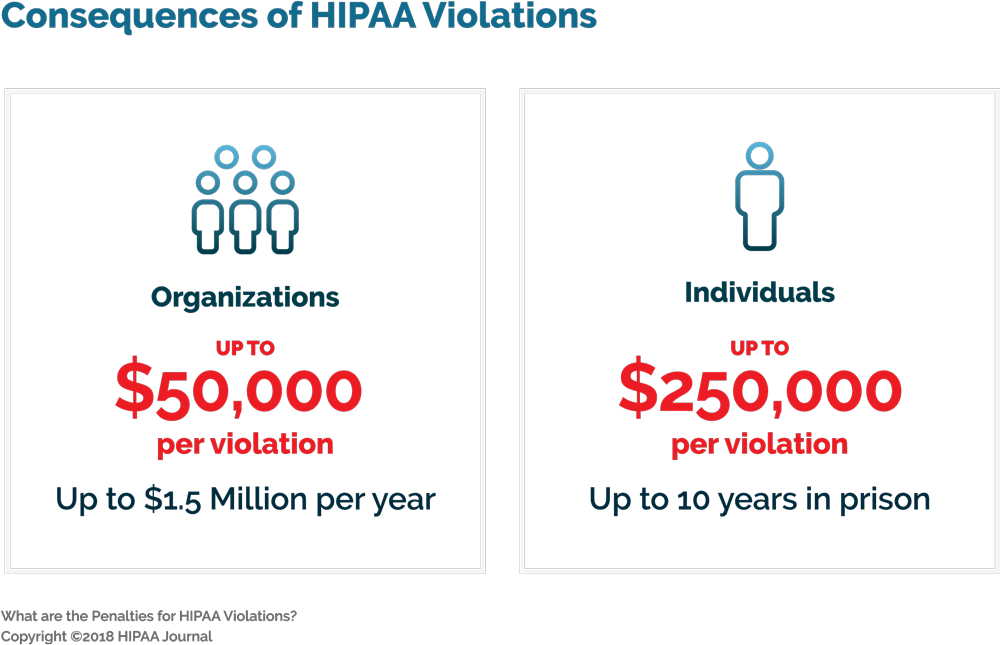
These risks are concerning, but what is the direct impact to healthcare providers when a breach occurs? HIPAA includes financial and criminal penalties for breaking the law’s rules on privacy and security. For healthcare organizations (HCO), each violation could cost as much as $50,000 in fines. Individuals could face fines up to $250,000 and up to 10 years in prison. These penalties have the potential to reach millions of dollars in cases involving many people’s PHI. Even if a breach is unintentional, the consequences can be severe. A provider must also consider downstream effects like damage to their reputation and loss of patient trust.
Other Important HIPAA Laws Pertaining to Telemedicine
HIPAA is not the only federal law that informs the proper handling of PHI. Many rules are crucial for providers to consider when using digital tools to handle patient data. These laws are also important to HIPAA compliant telehealth programs, as they update protections for the digital age.
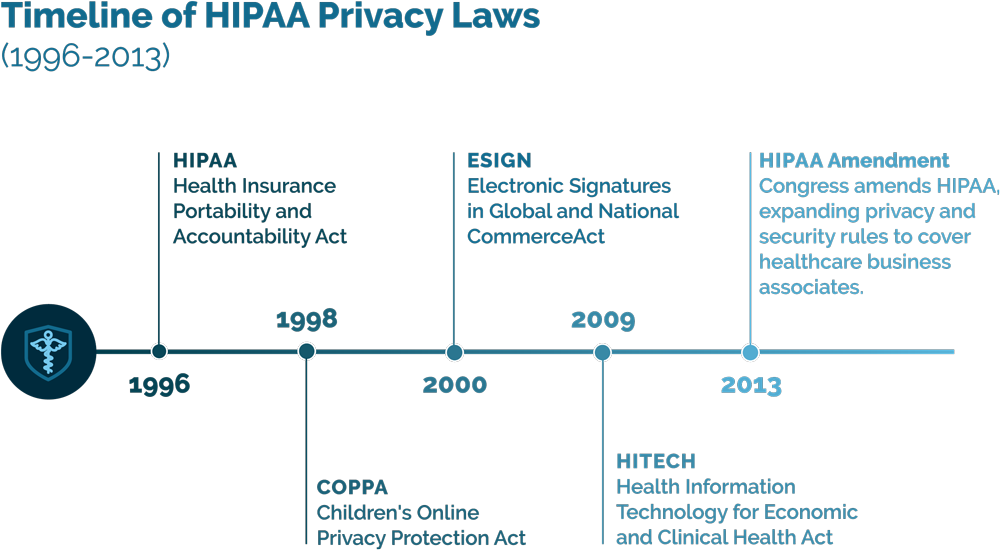
The Children’s Online Privacy Protection Act (COPPA) of 1998
COPPA sets rules for collecting data online on children under the age of 13. The law requires companies to inform parents or legal guardians on the use and sharing of children’s personal information. The intent of COPPA was to protect young people amid the rise of e-commerce and targeted online marketing. However, HCO’s must also comply with these rules when collecting and storing data on patients under 13 years old.
Electronic Signatures in Global and National Commerce (ESIGN) Act of 2000
The ESIGN Act set rules on collecting and confirming consent for electronic signatures. Telemedicine and HIPAA compliance permits collecting e-signatures in healthcare, but any process must comply with the ESIGN act. Of course, any method for storing e-signatures must also comply with HIPAA standard, just like any other PHI.
The Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009
The HITECH act strengthened HIPAA for the digital age. The intent of the law is increasing protections for PHI stored electronically, or ePHI. The law includes financial incentives for adopting safe and efficient EHR systems to manage patient data. Providers can also face added penalties for breaking HIPAA rules when handling ePHI.
Congress amended HIPAA itself in 2013, expanding privacy and security rules to cover healthcare business associates. The 2013 amendment pertains to vendors whose software handles PHI, making these HIPAA guidelines on telemedicine very relevant.
Keeping up-to-date with all of these crucial laws can feel overwhelming. However, there are public resources to help understand what these rules mean for you. Government agencies provide a great deal of material on the laws they enforce. Medical journals and other publications also publish articles to help the healthcare industry understand the laws that govern it. Take a look at some of these sources to learn more:
- HIPAA – Department of Health and Human Services (HHS)
- Children’s Privacy – Federal Trade Commission (FTC)
- HITECH Act Enforcement Interim Final Rule – Department of Health and Human Services (HHS)
- HIPAA Journal
HIPAA and Telehealth Platforms
The burden to protect PHI has only grown with the rise of web-accessible tools in healthcare. The same HIPAA rules apply to in-person healthcare and telehealth. With the challenge of cyberattacks growing, providers must look beyond their own conduct to promote security. They must also scrutinize how their software tools keep PHI secure.
Telehealth has become a very convenient method of care delivery for both patients and providers. However, this convenience can put PHI at risk if HCO’s don’t do their due diligence. Telehealth services rapidly expanded due to a dire need during the COVID-19 pandemic. This led to many providers choosing the fastest and simplest technology options. Video conferencing platforms like Zoom and Skype became popular for quickly starting a telehealth program.
However, standard video conferencing tools do not always include the security required with HIPAA compliance in telemedicine. The risks that come with a non-HIPAA compliant telehealth platform are high. Recent reports have revealed that Zoom will pay $85 million to settle a lawsuit for violating users’ privacy. These breaches include actively sharing user data with other firms and allowing hackers to access meetings. For any user, this negligence is troubling. However, for healthcare providers and their patients, it is dangerous.

What does great HIPAA Compliant Telehealth look like?
The Right Tools for High-Quality Telehealth
An encrypted video feed is a must to keep telehealth visits secure. However, that should not come at the expense of connection strength. Consider the bandwidth requirements of your software options. Encrypted video with a strong connection even at low bandwidths will provide both security and a positive user experience. With both high video quality and security, you can offer HIPAA compliant telehealth that is easy to use.
Providing Useful Instructions at a Distance
Even before a telehealth visit begins, providers can educate their patients to help make remote care run smoothly. The right telehealth software can help with notifications sent ahead of an appointment. Patient notifications should encourage pre-visit routines like preparing crucial information, testing connection speed, and securing their location. Instructions for connecting can make it easy for a patient to join their visit and keep their visit secure.
Providing an easy-to-understand user experience can also reduce security threats. Consider whether a platform requires patients to remember specific login data. Many patients have a dangerous habit of writing down usernames and passwords in unsecured locations. These credentials can be lost or stolen, creating vulnerabilities in your system. Verifying patient identities with a unique generated code for each visit reduces your dependence on their data privacy practices.
Some of these best practices may vary depending on the type of visit or the provider’s clinical specialty. That is why HIPAA compliant telehealth software should include customizable methods to notify patients based on a provider’s needs.
Secure the Provider and Patient Locations
Building a HIPAA compliant telehealth program goes beyond the technology itself. Providers must take their surroundings during a visit into account. Select a secure and quiet working location where only authorized individuals can see and hear the visit. Whether an office is in a commercial space or a home, it must be private.
Providers should separate themselves from staff, other patients, and anyone not essential to the visit. Sessions held in unfamiliar locations must be just as secure. If you cannot protect PHI in your current location, strongly consider whether you should reschedule a visit.
Likewise, the patient should also conduct their visit in a private location. Under HIPAA the patient is responsible for securing their own safe space for virtual treatment. Yet a provider can act as a valuable resource to help the patient protect their own privacy. A proactive approach to security can go a long way towards protecting patients and building trust. Here are some precautions that providers can take with patients when starting a telehealth visit:
- Have patients show you the room that they’re in to confirm privacy and identify potential security concerns.
- Identify anyone sharing the space with the patient. Confirm whether they have the patient’s permission to see or hear PHI.
- Confirm the address of the patient’s current location and match it with their address on file.
- Discontinue the session if the patient is not comfortable with the security of their current location.
These steps go beyond the requirements of HIPAA, but diligence is key to protecting your patients.
Adopt HIPAA Compliant Telehealth Software With Easy-To-Use Tools
The software you choose should be an asset to building a HIPAA compliant telehealth program, not a liability. A platform should encrypt communication channels and secure stored data. Providers have a responsibility to scrutinize the entire care environment, both physical and digital, to keep PHI secure. Equipping your workspace and care team to prioritize security is an important piece of the puzzle. Choosing a software partner that values security creates even more protection for you and your patients.
If you want to be confident that your telehealth services protect you and your patients, consider Mend. Mend is a total telehealth and patient engagement software that never compromises on security with all HIPAA compliant features. Mend is also SOC 2 Type 2 based on HITRUST, NIST CSF, HITECH Act, E-Sign Act, COPPA, ADA WCAG 2.0, PCI, CAN-SPAM, TCPA, & 42 CFR Part 2 compliant. Take advantage of high-quality video visits, automatic patient reminders, live tech support for patients and providers. Offer HIPAA compliant telemedicine with Mend, and use our suite of tools to help more patients than ever.