2022 Patient Payment Statistics and Bad Debt in Healthcare

Healthcare providers rely on getting paid in order to continue operating, and bad debt can have a significant impact on any business. Here are some of the most recent patient payment statistics as they relate to healthcare and what you can do as an organization to ensure timely payment.
What is Bad Debt in Healthcare?

What is bad debt in healthcare? It is money that is owed in medical billing to a healthcare provider but is not able to be collected. This happens for a variety of reasons, such as the patient not having insurance or not being able to pay their deductible. Bad debt can be a major financial burden for healthcare providers, as it can often be difficult or impossible to collect.
One of the most significant causes of bad debt is the increasing cost of patient financial responsibility. A recent report estimates the consumer out-of-pocket healthcare costs to reach $491.6 billion or about $1,650 per person by 2025.
What are Current Patient Payment Trends?
There are a few different trends for patient payments currently. As briefly mentioned above, one trend is that patients are increasingly responsible for a larger portion of their healthcare costs. As a result, patients are more likely to be looking for ways to save money on their healthcare costs.
Another trend is that more patients are using online payment options. This is because it is often more convenient and can help save time. Some online payment options also offer discounts. Or, they may offer lower prices than traditional methods like paying by cash or check.
Finally, there is a trend towards using alternative methods of payment, such as medical credit cards. This is because these cards can offer patients a way to finance their healthcare costs and pay over time. They can also often get patients discounts on their care.
Latest Statistics on Patient Payments
The latest patient payment statistics show that the average American household now owes more than $5,000 in medical debt. This is a significant increase from previous years, likely due to the rising cost of healthcare.
According to the same statistics, approximately one in five American households has “bad medical debt.” Hospital bad debt statistics translate to those payments that are over 90 days past due.
These numbers are concerning, as they indicate that many Americans are struggling with bad debt to make adjustments and keep up with their in medical bills.

How Many Healthcare Organizations Still Rely on Paper Bills
Even though most businesses have gone digital, many healthcare organizations rely on paper bills. In fact, 75% of providers primarily use paper and manual processes for payment collection.
As a result, this method can play a role in leading to bad debt for healthcare organizations. On average, it takes more than 30 days to collect after a patient encounter. To counter this, we can look at ways to improve the collection of patient payments in the future.
What Does the Future of Patient Payments Look Like?
The future of patient payments looks like it will be more electronic and automated. More and more, patients are using online tools to pay their bills and track their payments. This trend is likely to continue as the healthcare industry moves towards a more digitized system.
Consumers Want Digital Payment Options.
The InstaMed Annual Report shows an increasing interest from patients in digital payment options. The report found that 85% of consumers prefer an electronic payment method for their medical bills.
Another study shows patients aged 18 to 24 are three times as likely to consider switching providers over a poor digital experience.
Automatic digital payment processing
To stay competitive, patients want a modern, convenient patient engagement experience. Make patient payments easy and effortless, and organizations can get paid faster every time.
With the rise of telehealth comes more options for managing digital processes, including payment. For example, Mend’s digital check-in process handles patient co-pays, consents, digital forms, and more, automatically for both in-person and virtual visits.
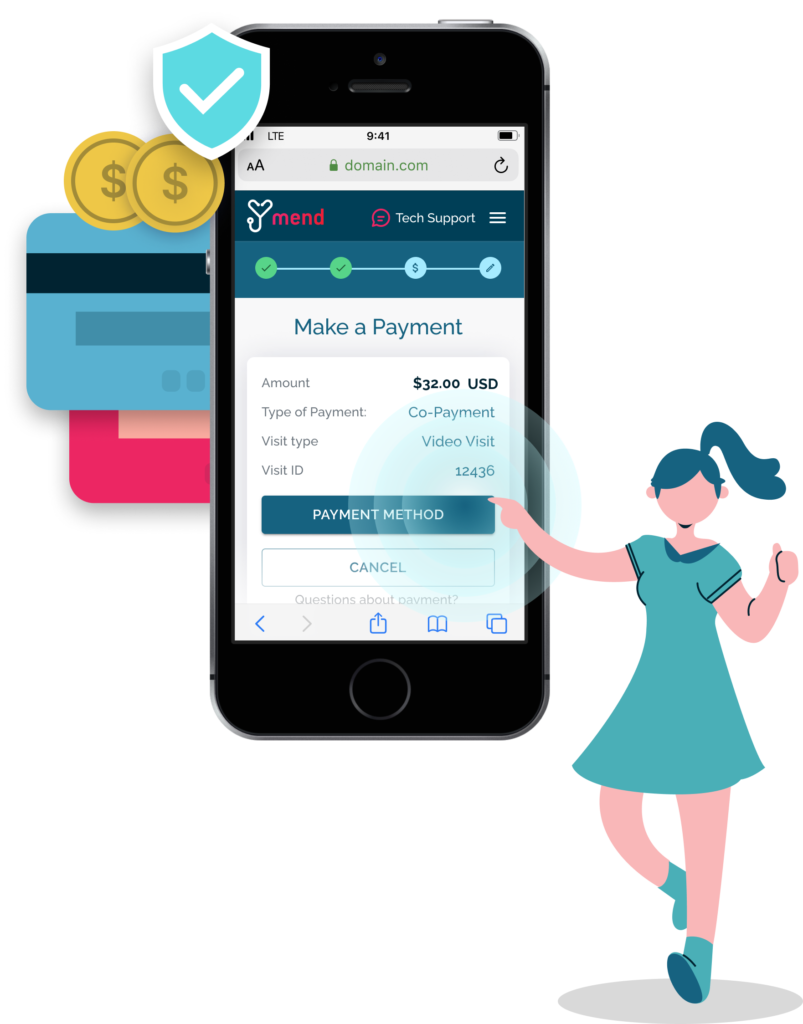
After a virtual visit is complete, the integration detects a positive patient balance. Mend can then automatically bill patient credit cards on file. Or, we can send a digital form invoice via text and email. Our management system quickly collects the amount due and then documents the payment.
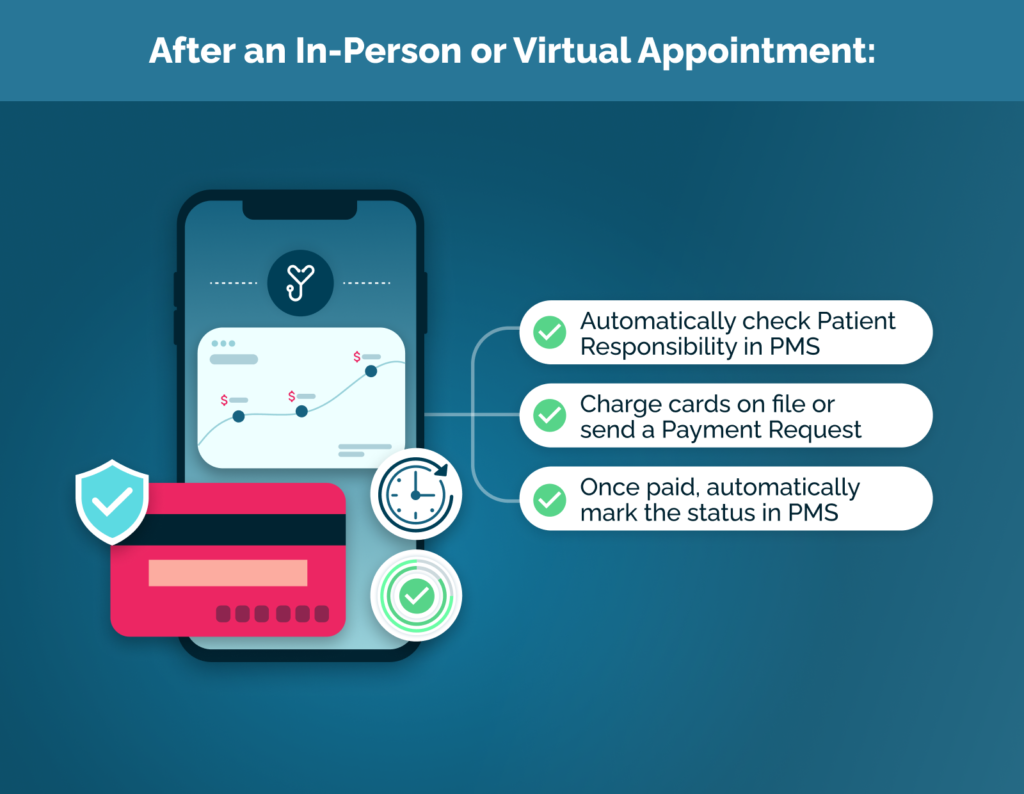
Automation of this process can also cut down on the cost of staffing. Paying staff to collect co-pays or chase patient balances after a visit is time-consuming and expensive.
How Has the Pandemic Affected Patient Payments?
The pandemic has had a significant impact on patient payments in healthcare. Many patients have lost their jobs or had their hours reduced. Twenty-nine percent of Americans lost their health insurance in 2020. Fifty percent of them remain uninsured in 2021. As a result, the average bad debt percentage in healthcare has increased significantly.
According to a Credit Karma survey, the finance company has seen its customers faced with an additional $3.6 billion in healthcare bad debt medical collections.
Tips for Prevention of Bad Debt
There are several ways that healthcare providers can prevent bad debt from occurring.
When it comes to bad debt medical billing, it is first essential to have a clear and concise billing policy in place. Patients have a right to transparent pricing and all costs related to their care before any treatment starts. This will help avoid misunderstandings about what the patient is responsible for paying.
Secondly, automating billing processes and offering digital patient payment options can provide a better overall patient financial experience in healthcare. It can also increase the speed of collection for providers. Mend already solves this by creating a digital check-in experience for in-person or virtual encounters. Patients can also store credit cards on file to charge automatically after the visit. Mend can also send an easy-to-use digital invoice that patients can pay electronically.
Lastly, it is also important to follow up with patients who have outstanding balances. Organizations need to contact patients soon after they receive their bill to remind them of the balance due. Providers can also offer payment plans to patients who are having trouble paying their bill in full.
Overall, there are several steps that healthcare providers can take to prevent bad debt from occurring. By having electronic payment options, a clear billing policy, and following up with patients, providers can help to ensure that patients are able to pay their bill in full.
Conclusion
There is no doubt that patient payment statistics and bad debt are major issues in healthcare. With the rising cost of healthcare, more and more patients are unable to pay their medical bills. This results in bad debt for healthcare providers, which can significantly impact their bottom line. However, there are steps that providers can take to reduce bad debt and improve patient payment statistics. By implementing effective billing and collection practices, providers can minimize the financial impact of these hospital bad debt trends.
FAQs
How do you collect payments from patients?
Payment collection can occur via digital or paper options, although more and more patients are requesting digital payment options. Automated payment processing and the acceptance of digital payment both contribute to the speed of collection. Ideally, a medical practice should bad debt by collecting payments before or at the time of service.
Who is responsible for collecting patient payments?
The responsibility for collecting patient payment falls to the practice or organization. This is why practices need to make the payment processing process as smooth as possible. An integrated payment processing system that accepts digital payment options can increase speed to collection. Outsourcing difficult collections to vendors can reduce the manual hours of the front desk staff.
What are the different types of payment systems in healthcare?
In a fee-for-service (FFS) model, physicians receive payment for each individual service they provide to patients. With capitation, the physician receives a set amount per patient per a given period of time. Episode-based payments pay providers the same rate for standard procedures. For example, if a physician performs hip surgeries, they will receive the same amount for each surgery although some will cost more and some will cost less.
Keyword:
Find a Topic:
Recent Posts
- Compassionate Foundations: Self-Care for Mental Health Providers
- Behavioral Health News: Mend Partners with Leading Community Mental Health Organizations to Reduce No-Shows and Increase Access to Care
- Understanding SAMHSA’s Key Changes to 42 CFR Part 8: A Guide for Healthcare Professionals
- Becoming a CCBHC: Staffing Requirements
- Empowering Change: SAMHSA’s Impact on Behavioral Health Through Grant Funding, Innovation, and Collaboration